Advancing Healthcare by Empowering Women in Emergency Medicine
Advancing Healthcare by Empowering Women in Emergency Medicine
Advancing Healthcare by Empowering Women in Emergency Medicine
Together, we will improve the careers of women practicing emergency medicine while facilitating better care for our patients.
Together, we will improve the careers of women practicing emergency medicine while facilitating better care for our patients.
Together, we will improve the careers of women practicing emergency medicine while facilitating better care for our patients.
Leadership Development
Leadership Development
Leadership Development
Our leadership programs empower women in emergency medicine to develop the skills and confidence needed to advocate for themselves and their patients.
Our leadership programs empower women in emergency medicine to develop the skills and confidence needed to advocate for themselves and their patients.
Our leadership programs empower women in emergency medicine to develop the skills and confidence needed to advocate for themselves and their patients.
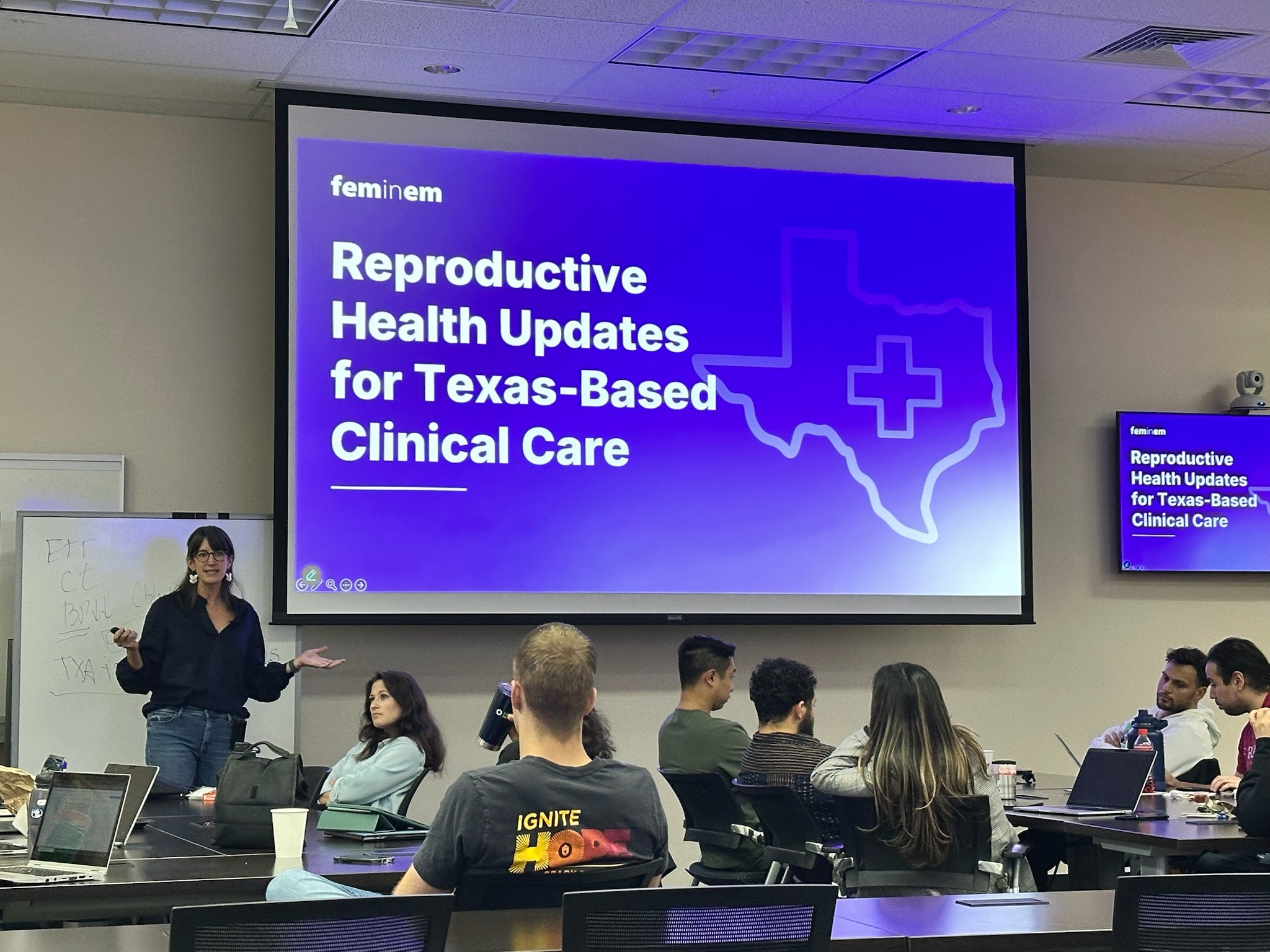
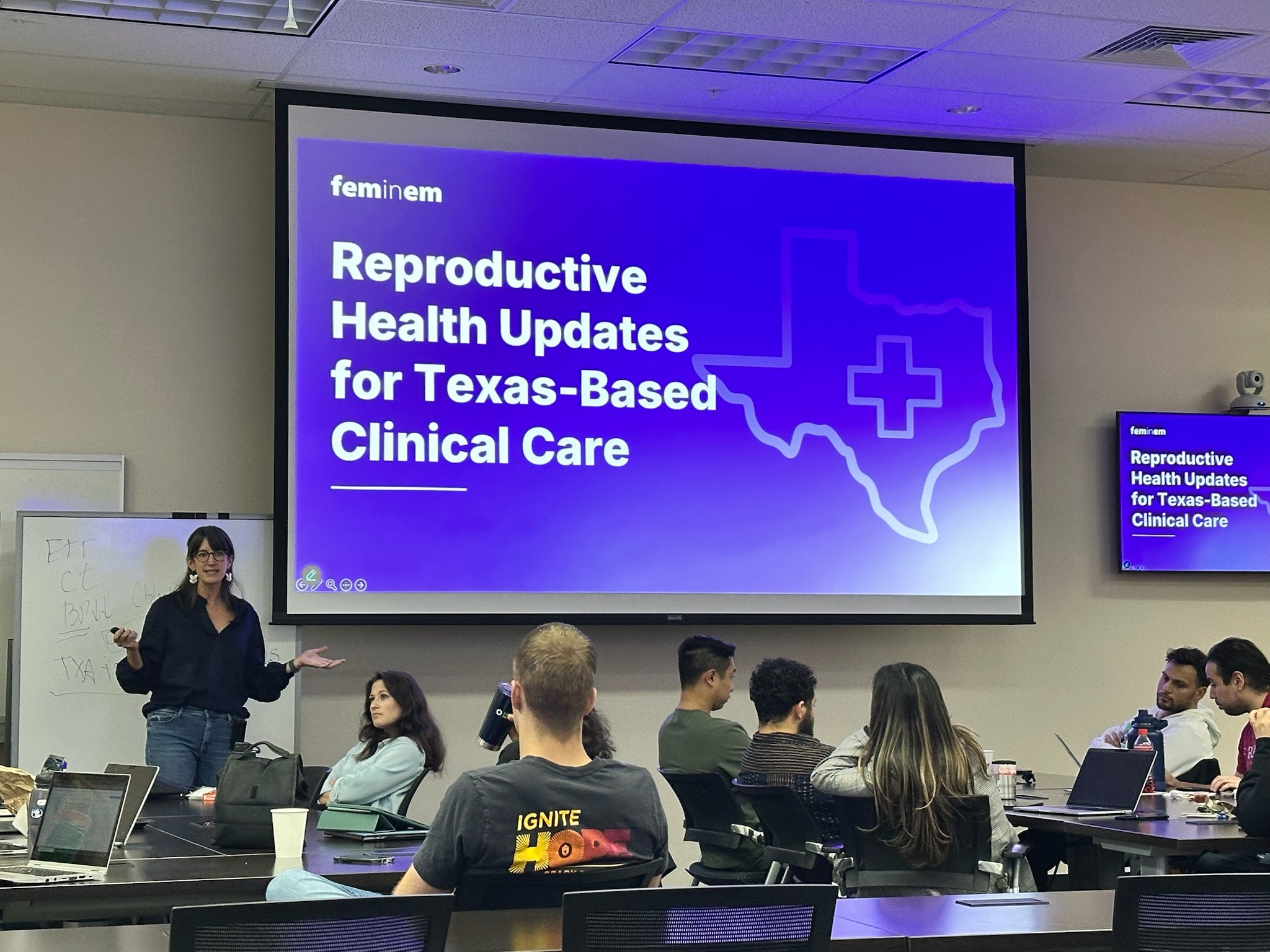
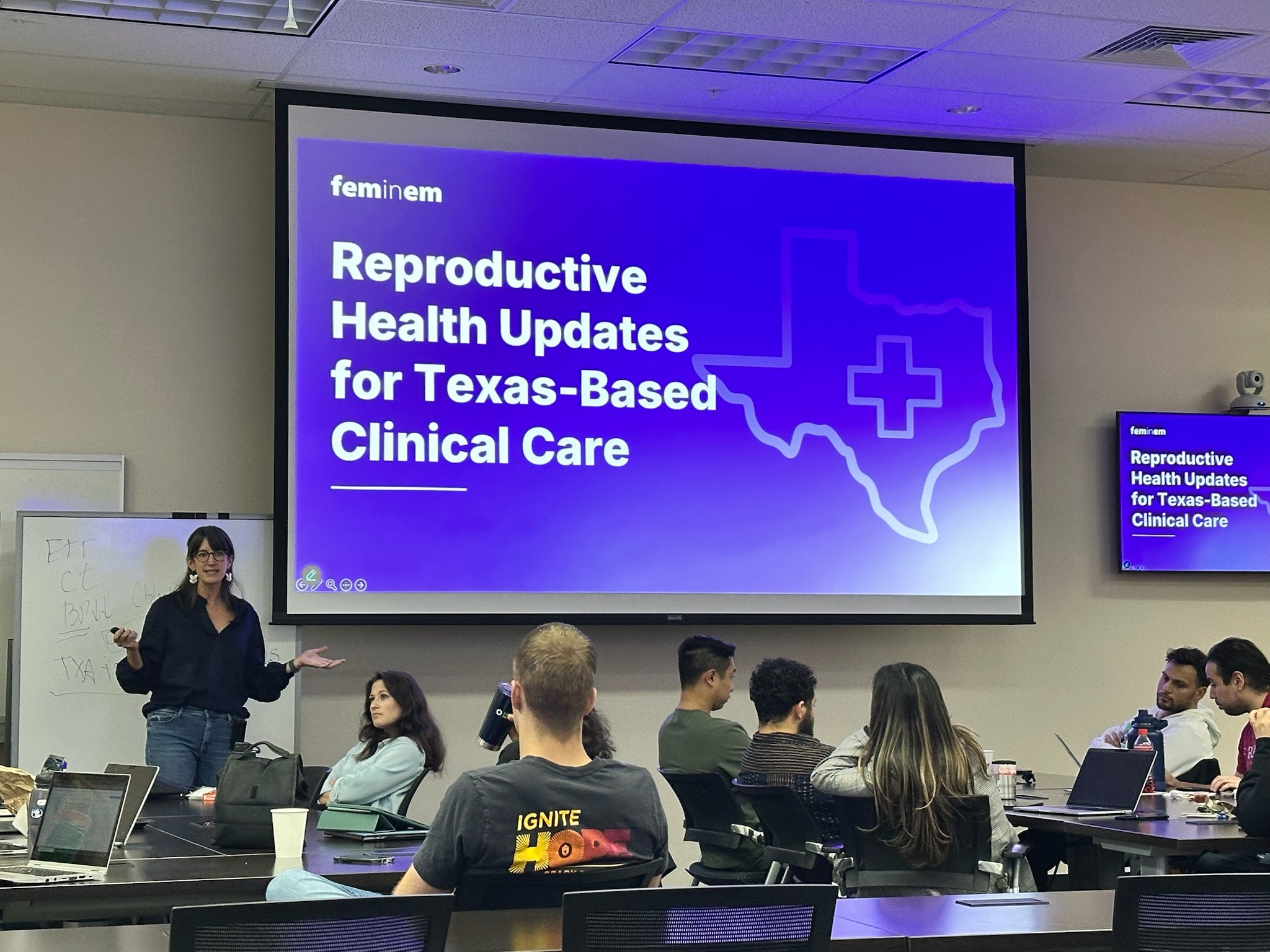
Clinical Education
Clinical Education
Clinical Education
Our clinical education resources are designed to ensure that all patients, especially women, receive evidence-based care in emergency departments across diverse settings.
Our clinical education resources are designed to ensure that all patients, especially women, receive evidence-based care in emergency departments across diverse settings.
Our clinical education resources are designed to ensure that all patients, especially women, receive evidence-based care in emergency departments across diverse settings.
Research & Collaboration
Research & Collaboration
Research & Collaboration
We champion research and collaboration focused on advancing gender equity and reproductive healthcare in emergency medicine.
We champion research and collaboration focused on advancing gender equity and reproductive healthcare in emergency medicine.
We champion research and collaboration focused on advancing gender equity and reproductive healthcare in emergency medicine.


Speakers
Speakers
Speakers
CME Hours Delivered
CME Hours Delivered
CME Hours Delivered
Learners Across 12 States
Learners Across 12 States
Learners Across 12 States
Explore Our Substack
Explore Our Substack
Explore Our Substack
An additional hub for our stories, news, and resources that helps us do our work in the ED and at home.
An additional hub for our stories, news, and resources that helps us do our work in the ED and at home.
An additional hub for our stories, news, and resources that helps us do our work in the ED and at home.
Speaker Bureau
Speaker Bureau
Discover a diverse network of seasoned experts ready to share insights on topics from leadership and wellness to trauma care and public health.
Book a speaker — or join the roster yourself!
Discover a diverse network of seasoned experts ready to share insights on topics from leadership and wellness to trauma care and public health.
Book a speaker — or join the roster yourself!
Discover a diverse network of seasoned experts ready to share insights on topics from leadership and wellness to trauma care and public health.
Book a speaker — or join the roster yourself!
Programs
Programs
for Everyone Practicing Emergency Medicine
for Everyone Practicing Emergency Medicine
for Everyone Practicing Emergency Medicine
Physician Outreach & Education Program
Physician Outreach & Education Program
Physician Outreach & Education Program
Supporting Emergency Department Physicians to deliver compassionate, legally sound, and clinically excellent care — and growing beyond.
Supporting Emergency Department Physicians to deliver compassionate, legally sound, and clinically excellent care — and growing beyond.
Supporting Emergency Department Physicians to deliver compassionate, legally sound, and clinically excellent care — and growing beyond.



Champions of Change Leadership Program for Medical Students
Champions of Change Leadership Program for Medical Students
Champions of Change Leadership Program for Medical Students
Through specialized training modules, we equip students with leadership, advocacy, and practical tools to improve reproductive healthcare.
Through specialized training modules, we equip students with leadership, advocacy, and practical tools to improve reproductive healthcare.
Through specialized training modules, we equip students with leadership, advocacy, and practical tools to improve reproductive healthcare.
Reproductive Health Care (RHC) Working Groups
Reproductive Health Care (RHC) Working Groups
Reproductive Health Care (RHC) Working Groups
Brings together emergency physicians in similar practice environments to exchange best practices and develop regionally tailored strategies.
Brings together emergency physicians in similar practice environments to exchange best practices and develop regionally tailored strategies.
Brings together emergency physicians in similar practice environments to exchange best practices and develop regionally tailored strategies.



Resources
Resources
Strengthen Your Clinical Practice and Advance Your Professional Growth
Strengthen Your Clinical Practice and Advance Your Professional Growth
Strengthen Your Clinical Practice and Advance Your Professional Growth
Clinical Resources
Clinical Resources
Clinical Resources
Evidence-based protocols that equip physicians to manage reproductive health emergencies and ensure optimal patient outcomes.
Evidence-based protocols that equip physicians to manage reproductive health emergencies and ensure optimal patient outcomes.
Evidence-based protocols that equip physicians to manage reproductive health emergencies and ensure optimal patient outcomes.
Promotion & Development Resources
Promotion & Development Resources
Promotion & Development Resources
Equips women physicians with actionable strategies for work-life balance, leadership development, and gender equity to thrive and lead in emergency medicine.
Equips women physicians with actionable strategies for work-life balance, leadership development, and gender equity to thrive and lead in emergency medicine.
Equips women physicians with actionable strategies for work-life balance, leadership development, and gender equity to thrive and lead in emergency medicine.
Stay Informed. Stay Ahead.
Stay Informed. Stay Ahead.
Stay Informed. Stay Ahead.
Get the latest clinical tools, professional development opportunities, and expert insights — delivered straight to your inbox.
Get the latest clinical tools, professional development opportunities, and expert insights — delivered straight to your inbox.
Get the latest clinical tools, professional development opportunities, and expert insights — delivered straight to your inbox.


Donate
Donate
Give To this vital work
Give To this vital work
Give To this vital work
Your generosity keeps us going. Help make a difference in reproductive healthcare in emergency medicine.
Your generosity keeps us going. Help make a difference in reproductive healthcare in emergency medicine.
Your generosity keeps us going. Help make a difference in reproductive healthcare in emergency medicine.
FemInEM recognizes the enormous leadership potential of women with emergency medicine training. Unlike other professional society meetings and leadership programs I've attended, the FemInEM conference was about making an impact on people in your community and globally by bringing your whole self as a woman and leader to the table...we're women who show up for others to ignite ideas, grow programs, and improve the world around us!
Dr. Liz Goldberg
Denver, Colorado
FeminEM advocates for more research to inform the care of women. Specifically to improve reproductive healthcare delivery in emergency departments. Women deserve the best care, based on the best evidence.
Dr. Ken Milne
London, Ontario
It was after attending my first FeminEM retreat I felt I finally found my tribe in emergency medicine. Here was a safe place to share our unique struggles, genuinely celebrate our victories, and collaborate to improve the culture of emergency medicine for other female physicians.
Dr. Breanne Jacobsilne
Washington, D.C.
In my second year of residency, I mustered up the courage to tell one of my APDs that I wanted to be an abortion provider. I felt super scared telling anyone this or saying it aloud for the first time...Pretty amazing to think this was actually the seed that was planted for me, in retrospect.
Anonymous EM Physician
Anonymous
FemInEM has been a lifeline in the storm of emergency medicine, where burnout is staggering, especially among women. This organization uniquely bridges professional development, peer support, and advocacy, tackling the root causes of moral injury and burnout that drive women from our field. By empowering women to reclaim their careers and well-being, FemInEM transforms clinicians' lives and enhances the care we provide, ultimately benefiting the patients we serve.
Dr. Andrea Austin
San Diego, California
FemInEM recognizes the enormous leadership potential of women with emergency medicine training. Unlike other professional society meetings and leadership programs I've attended, the FemInEM conference was about making an impact on people in your community and globally by bringing your whole self as a woman and leader to the table...we're women who show up for others to ignite ideas, grow programs, and improve the world around us!
Dr. Liz Goldberg
Denver, Colorado
FeminEM advocates for more research to inform the care of women. Specifically to improve reproductive healthcare delivery in emergency departments. Women deserve the best care, based on the best evidence.
Dr. Ken Milne
London, Ontario
It was after attending my first FeminEM retreat I felt I finally found my tribe in emergency medicine. Here was a safe place to share our unique struggles, genuinely celebrate our victories, and collaborate to improve the culture of emergency medicine for other female physicians.
Dr. Breanne Jacobsilne
Washington, D.C.
In my second year of residency, I mustered up the courage to tell one of my APDs that I wanted to be an abortion provider. I felt super scared telling anyone this or saying it aloud for the first time...Pretty amazing to think this was actually the seed that was planted for me, in retrospect.
Anonymous EM Physician
Anonymous
FemInEM has been a lifeline in the storm of emergency medicine, where burnout is staggering, especially among women. This organization uniquely bridges professional development, peer support, and advocacy, tackling the root causes of moral injury and burnout that drive women from our field. By empowering women to reclaim their careers and well-being, FemInEM transforms clinicians' lives and enhances the care we provide, ultimately benefiting the patients we serve.
Dr. Andrea Austin
San Diego, California




